What is Hip Arthroscopy (Key hole Surgery)?
An arthroscope is a small telescope that allows the surgeon to investigate and treat a joint without making a large incision. The part of the scope that is inserted into the joint is roughly the same size and length as a pencil. The telescope is attached to a small video camera allowing the surgeon to visualize the joint on a TV screen.
How are instruments placed into the hip joint?
The patient is positioned on their back on the operating table and anesthesia is given. Traction is applied to the patient’s leg until 1-2 cm of space is created between the hip ball and hip socket allowing the insertion of instruments to proceed without damage to the surrounding joint. Two or 3 puncture holes about 1 cm in size are generally needed in order to complete the surgery. Small instruments such as graspers, shavers and cutters are introduced through these puncture hole in order to work on the hip.
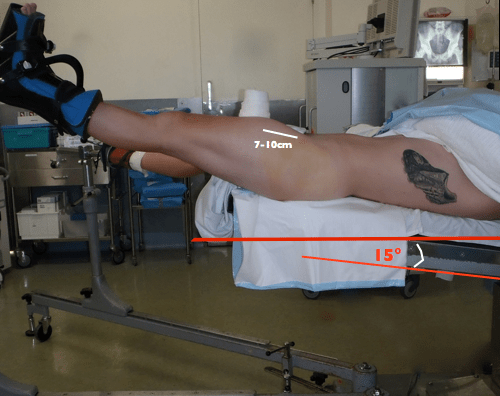
Patient positioned for surgery

The sterile drapes in place with instruments inserted
Does arthroscopic surgery work?
Success rates in the published literature, in appropriately selected patients, show 80 or 90% of patients experience a substantial improvement in pain and most are able to return to sports. Patients with mild to moderate arthritis are not good candidates for this operation. We do not know what the long term effect of hip arthroscopy will be on the hip. We are hopeful that having early repair of abnormal hip anatomy may prevent some hip arthritis down the road. Studies able to demonstrate whether this is possible are at least 10 years away.
Below is a representation of the outcome scores seen in patients who underwent hip arthroscopy in New Zealand during my hip arthroscopy training. Further research that I have published from New Zealand and from other collaborative work supports these good short to medium term results. Keep in mind these results are in well selected patients that are appropriate for hip arthroscopy.
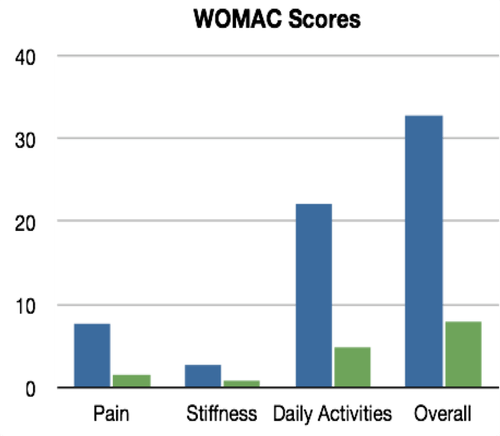
Blue is preoperative and green is 6 months postoperative. A lower score is better.
Post Operative
The patient is able to go home the same day and can usually weight bear immediately with crutches. Patients use crutches for between 2-6 weeks depending on the type of surgery they had and until they can walk without a limp.
Return to Work – One to 2 weeks off of desk type work is likely required. If the job was very physical such as a construction worker or builder, 2 or 3 months off work may be required.
Physiotherapy – Physiotherapy will be necessary in the postoperative period. Using a stationary bicycle is an excellent form of early rehabilitation and can be started as early as 1-3 days post-op. Your physiotherapist will teach you exercises to strengthen the hip muscles and the core muscles (abdominal and back muscles) as well as a stretching program. Time back to sports is more commonly 3 to 4 months.
Pain Management – How painful the postoperative period is for each patient depends on the surgery involved and the patient’s response to pain. Everyone is different. Having said that, after the first few days most people are relatively comfortable. Your surgeon will provide you with a prescription for pain medication. Icing can also help and a cryocuff can be very useful to help decrease swelling and pain.

During the 12 week early healing phase the patient may be completely comfortable while walking, sitting or lying, but get a sharp jab of pain with a sudden twisting movement. This is likely stretching the healing capsule. An example would be trying to do a breaststroke kick in a swimming pool two weeks post-op would almost certainly be painful. Swimming freestyle, however, would likely be more comfortable.
Medications – Patients may need some strong analgesics for the first few days but can usually switch to medications like Tylenol and Advil relatively quickly.
Exercise – Will I be able to run or play sports again? In most cases the answer to this question is yes. The damage in some patients is significant enough at the time of surgery that impact activities, such as running, may not be advisable after a hip operation. If this is suggested it is in an attempt to prolong symptom free function and avoid further degeneration of the hip.
Long Term – Will this surgery stop osteoarthrosis and the future need for a hip replacement? Hip preservation surgeons certainly hope that by changing the abnormal anatomy of the hip to avoid repetitive damage to the joint surface the risk of arthritis may be diminished. However, no data is available to support these claims at this time. Scientific evidence is at least ten years away before any such claim can be made.
Risks & Complications
Traction injuries – The traction boot can cause pressure areas on the ankle or the heel and also around the genital area in women and behind the scrotum in men (the perineum). The nerves to the genitals can be compressed. A small minority of patients will experience numbness in their groin (around their genitals) if a post was used but if it does occur typically dissipates over a few days to weeks.
Numbness to the thigh – There is a nerve that runs close to the incisions that are made around the hip for hip arthroscopy. Its sole function is to give sensation to the skin of the thigh. Branches of this nerve can be stretched or irritated during hip arthroscopy. Most often if there is some numbness it resolves on its own in the first few days or weeks after surgery.
Anaesthetic complications – In a healthy person a modern general anaesthetic is very safe. Situations such as adverse reactions to drugs or airway issues can be very serious but fortunately are very unusual.
Stress fracture – By removing bone from the femoral neck, theoretically the femoral neck is weakened. Returning to impact activities too quickly can put the patient at risk for a stress fracture. Even when crutches are not needed a return to impact activities should not occur prior to 10-12 weeks.
Avascular necrosis of the femoral head – This is perhaps the worst complication but fortunately is extremely rare. At the time of arthroscopic surgery great care is taken to avoid the blood vessels that supply blood to the femoral head. Disruption of the blood supply to the femoral head often leads to death of that part of the bone and often necessitates a hip replacement. There have only been a few cases of this complication reported in the scientific literature out of the tens of thousands of hip arthroscopic procedures that have been performed around the world.
Adhesive capsulitis – In the postoperative period patients can get a stiff hip as a result of the inflammation associated with healing. This usually manifests sometime between eight and twelve weeks post-op. The healing capsule becomes thick, tight and inflamed. The patient feels as though they are making good progress but then gradually the hip becomes more restricted and painful. A cortisone injection into the hip may help relieve the symptoms if indeed adhesive capsulitis occurs.
Infection – Infections are very rare after arthroscopic surgery of any joint because so much fluid is washed through the joint during the procedure. No good percentage numbers are available for hip arthroscopy but certainly would be less than 1/200-500. The wound will drain some clear to bloody looking fluid over the first few days. Pink solution is used to clean the skin and can sometimes be confused with redness. Increasing discharge after the first few days, foul smelling discharge, fevers and sweats or increasing hip pain are some of the signs of infection that should alert the patient to seek medical treatment.
Blood Clot (Deep Vein Thrombosis) – After any lower extremity surgery the patient is at risk of developing a blood clot in the large veins of their leg. It is unusual after hip arthroscopy but still may present in up to 1% of patients. The signs of a blood clot include a warm, swollen painful calf. The blood clot can move to the lungs and cause the patient to be very sick and in rare cases it can be fatal. Again this is a rare complication of any surgery of the leg but one that patients should be aware of. An ultrasound can be ordered to rule out a blood clot if there are signs and symptoms warranting this investigation.
The above list is not comprehensive but serves as a guide to some of the risks of this or any surgery. Hip arthroscopy is very safe but being well informed about the surgery can help in a patient’s recovery and improve the anxiety around an operation.

The cam lesion is seen at the junction of the femoral head and neck.

This post-op CT scan no longer shows a cam lesion.
